Part 4: Some Gastroenterologists Still Don't Believe
That Non-Celiac Gluten Sensitivity Exists

This article describes one of six things I've learned about gastroenterologists through my personal experiences and through research. I'd suggest you set your expectations accordingly, but your experiences might vary from mine.
In this article, I provide examples showing that some gastroenterologists still don't believe in the existence of non-celiac gluten sensitivity (often shortened to “gluten sensitivity”).
For the complete series of articles, see Six Things You Should Know About Gastroenterologists.
A Question Some Gastroenterologists Ask of Other Doctors: “Why Did You Put This Patient on a Gluten-Free Diet? She Doesn’t Have Celiac Disease.”
 People with non-celiac gluten sensitivity tend to suffer from non-GI symptoms such as headache, “foggy mind,” behavioral changes, fatigue, bone or joint pain, and numbness in the extremities. (1)
People with non-celiac gluten sensitivity tend to suffer from non-GI symptoms such as headache, “foggy mind,” behavioral changes, fatigue, bone or joint pain, and numbness in the extremities. (1)Neurologist David Perlmutter, author of Grain Brain, shares a story on his web site about treating a patient who had a history of headaches for 40 years. He writes:
“I did some blood work and found that she was gluten sensitive. I took her off of gluten and her headaches went away. She then visited with her gastroenterologist who picked up the phone and called me and said 'Why did you put this patient on a gluten-free diet? She doesn’t have celiac disease.' I began to explain about something called non-celiac gluten sensitivity and I have to admit there was a lot of silence on the other end of the phone. There are still a lot of people that don’t believe that there really is such a thing as being gluten sensitive if you don’t have celiac disease.” (2)
If testing reveals that you don't have celiac disease, consider the possibility of non-celiac gluten sensitivity—even if your gastroenterologist (or your family doctor) doesn't. You could eliminate gluten from your diet for a month or two and see what happens. If your symptoms improve, chances are you do have non-celiac gluten sensitivity.
My nephew was diagnosed with Crohn's disease at age 16. His gastroenterologist tested him for celiac disease, and the results showed no signs of it. However, this doctor did not explore the possibility of non-celiac gluten sensitivity. He did not suggest that my nephew try a gluten-free diet to see if his symptoms might improve.
I'm not declaring that gluten causes all cases of Crohn's disease, but it could be one of the environmental triggers for it, at least for some people.
Besides, if someone is having serious digestive problems, how could eating gluten—which no human on this planet can properly digest—possibly facilitate healing? And why don't gastroenterologists know this?
Let me repeat myself: No human on this planet can properly digest gluten. Am I an anti-gluten fanatic, or is this statement really true? Do any gastroenterologists believe this to be true?
During an interview with Alessio Fasano, MD, a pediatric gastroenterologist and celiac disease researcher, the interviewer, Elisabeth Veltman from The Tender Foodie blog, was surprised to hear Dr. Fasano make this statement. In fact, she asked for clarification.
“That sounds like everyone is gluten intolerant in some way. Is that true? Everyone?” she asked.
“Yes,” said Dr. Fasano. “No one can properly digest gluten. We do not have the enzymes to break it down.”
He explained that whether we develop celiac disease, non-celiac gluten sensitivity, or gluten/wheat allergy “depends upon how well our intestinal walls close after we ingest [gluten] and how our immune system reacts to it.” (3)
Evidently, most people have intestinal walls that close after they ingest gluten, and their immune system doesn't start a war over the infraction. But, unfortunately, a good number of us do have this outcome.
A Case Study of Non-Celiac Gluten Sensitivity and Crohn's Disease

A case study of a male patient published in the peer-reviewed journal Case Reports in Immunology (4) demonstrates the association of non-celiac gluten sensitivity with Crohn's disease.
As the authors state in their discussion of this case, “It is contemplated herein that continuous exposure to environmental factors, such as wheat antigen-induced inflammation for a prolonged period of time, may result in inflammatory bowel disease or Crohn’s disease.”
Here's a summary of the details:
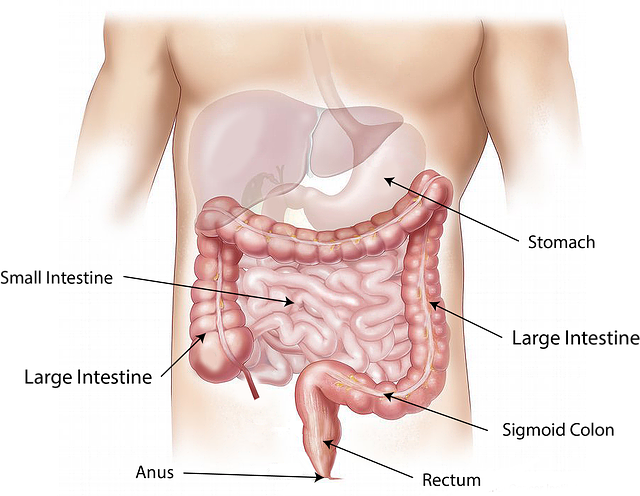
A male patient had worsening gastrointestinal discomfort and diarrhea, as well as a loss of 12 pounds of his body weight, over three years after which he was diagnosed with Crohn's disease. Two years of multiple treatments for this disease failed to help, and he ended up having 22 centimeters of his ileum (lower small intestine) removed.
This patient continued to suffer an additional eight years during which he endured an increasing frequency of diarrhea and an additional loss of 14 pounds. Finally, he was tested for non-celiac gluten sensitivity using a comprehensive IgG and IgA panel against an array of wheat proteins and peptides.
Results showed the patient had a significant elevation of IgG antibodies against 11 out of 12 tested antigens, as well as a significant elevation of IgA antibodies against 6 of these antigens.
Due to these results, the patient was given the additional diagnosis of non-celiac gluten sensitivity. After six weeks on a gluten-free (and yeast-free) diet, his diarrhea stopped—completely. After one year, he was back to normal and had regained more than 80% of the weight he had lost.
Sadly, this diagnosis of non-celiac gluten sensitivity could have been made 14 years earlier when this patient had been tested for IgG antibodies against gliadin. Results showed his antibodies were moderately elevated at 59 U/mL (normal value ≤ 20 U/mL). Unfortunately, the IgG antibody elevations were considered “nonspecific or protective.” The patient was placed on painkillers and sent home without a diagnosis.
The authors discuss how this patient's disease process could have been initiated by non-celiac gluten sensitivity, not Crohn's disease.
I would state more directly: Had this patient been diagnosed with non-celiac gluten sensitivity 14 years earlier and had he immediately gone gluten free, very likely he never would have developed Crohn's disease.
The Story of a Young Woman With Undiagnosed Gluten Sensitivity Whose Entire Colon Was Surgically Removed
 A total abdominal colectomy removes the large intestine from the ileum (lower small intestine) to the rectum. Then, the end of the small intestine is sewn to the rectum.
A total abdominal colectomy removes the large intestine from the ileum (lower small intestine) to the rectum. Then, the end of the small intestine is sewn to the rectum.My former psychotherapist had a client who was diagnosed with Crohn's disease. This young woman, who was a teenager at the time of her diagnosis, was told by her gastroenterologist that she had a mild case and that medications typically prescribed for Crohn's would manage her disease well.
Despite faithfully following doctor's orders, her disease progressed rapidly over a few years' time. She endured multiple surgeries to remove parts of her large intestine, but her disease continued to devastate her body. In the end, her entire large intestine was surgically removed.
Even after all those invasive surgeries, this woman still felt sick...
On her own, she embarked on a gluten-free diet, and her remaining symptoms quickly improved. She feels good again—except, of course, she is forever missing her large intestine and must deal with the consequences for the rest of her life.
Not surprisingly, all those conventional medical treatments for Crohn's disease traumatized her. That's why she pursued psychotherapy: to help heal that trauma.
Had her gastroenterologist recommended early on that she try a gluten-free diet, might she have avoided all of this misery? How can one not wonder...
References
1. Sapone A, Bai, JC, Ciacci C, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Medicine. 2012, 10:13.
2. Perlmutter, D. Understanding Gluten Sensitivity. Blog post dated Oct 5, 2014.
3. Veltman E. Interview W/ Dr. Alessio Fasano, Part 1: Should Anyone Eat Gluten? The Tender Foodie blog. Dec 19, 2011.
4. Vojdani A, Perlmutter D. Differentiation between Celiac Disease, Nonceliac Gluten Sensitivity, and Their Overlapping with Crohn’s Disease: A Case Series. Case Reports in Immunology. 2013. Article ID 248482, 9 pages.
CeliacFAQ.com home page > Articles >
6 Things You Should Know About Gastroenterologists > Some Gastroenterologists Deny Non-Celiac Gluten Sensitivity